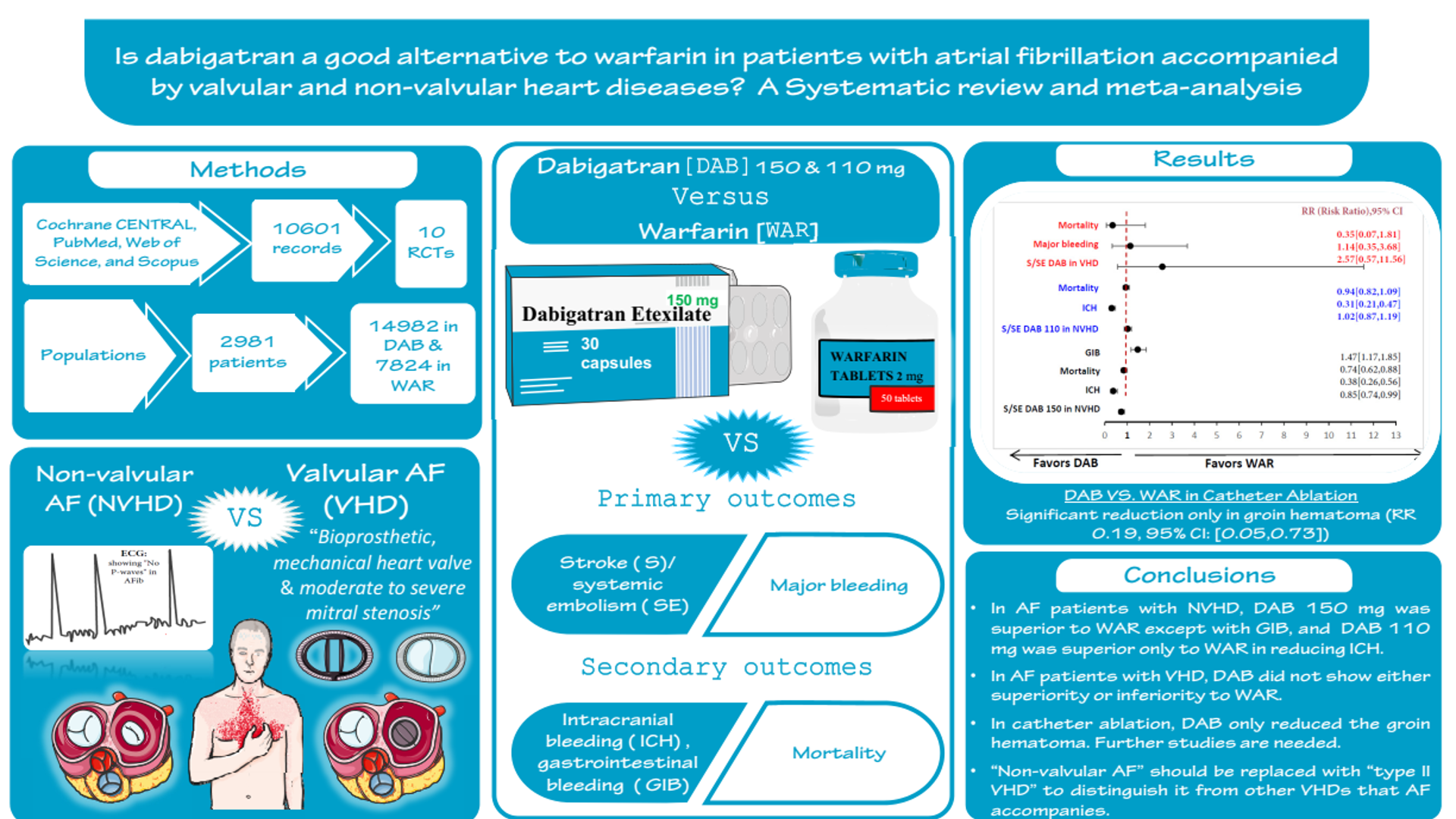
Is dabigatran a good alternative to warfarin in patients with atrial fibrillation accompanied by valvular and non-valvular heart diseases? A systematic review and meta-analysis
##plugins.themes.academic_pro.article.main##
Abstract
Background: There is ongoing discussion regarding the terminology used when atrial fibrillation (AF) is present alongside either valvular heart disease (VHD) or non-valvular heart disease (NVHD). We conducted this meta-analysis to assess the effectiveness and safety of dabigatran compared to warfarin in AF patients with VHD and NVHD.
Methods and results: Online databases were searched for eligible studies. Ten RCTs (22981 patients) were included. In NVHD subgroup, dabigatran 150 mg showed no statistically significantly difference in stroke (S) and systemic embolism (SE) (risk difference (RD) -0.01,95% confidence interval(CI):-0.01,0.0), and death (RD -0.00,95% CI -0.01,0.00) except for intracranial hemorrhage (ICH) (RD -0.01,95% CI -0.01,-0.01), and major bleeding (RD -0.02,95% CI -0.04,-0.00), similarly ,110 mg showed a low risk of ICH (RD -0.01,95% CI -0.01,-0.01), and no significant differences in S/SE and death compared to warfarin. In VHD subgroup, dabigatran showed no significant differences in S/SE (RD 0.02,95% CI -0.03,0.07), major bleeding (RD 0.01,95% CI -0.02,0.04), and death (RD -0.01,95% CI -0.04,0.01) compared to warfarin. In the catheter ablation subgroup, dabigatran reduced only groin hematoma (RD -0.02,95% CI -0.03,-0.00).
Conclusion: Dabigatran 150 mg and 110 mg was superior to warfarin in AF patients with NVHD in reducing bleeding particularly ICH; However, no significant difference in reducing S/SE, and mortality. In catheter ablation, dabigatran reduced only groin hematoma. In the VHD subgroup, dabigatran did not show superiority or inferiority to warfarin; further studies are needed. “Non-valvular AF” should be replaced with “type II VHD” to distinguish it from other valvular heart diseases.
Keywords:
Catheter ablation, Dabigatran, Non-valvular atrial fibrillation, Valvular atrial fibrillation, Warfarin##plugins.themes.academic_pro.article.details##

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
- Calkins H, Hindricks G, Cappato R, et al (2018) 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace 20:e1–e160
- Ohlrogge AH, Brederecke J, Schnabel RB (2023) Global Burden of atrial fibrillation and flutter by national income: Results from the Global Burden of Disease 2019 database. J Am Heart Assoc 12:e030438
- Kirchhof P, Benussi S, Kotecha D, et al (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 37:2893–2962
- Avezum A, Lopes RD, Schulte PJ (2015) Apixaban in comparison with warfarin in patients with Atrial Fibrillation and valvular heart disease: Findings from the apixaban for Reduction in stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial: Findings from the apixaban for Reduction in stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial. Circulation 132:624–632
- Fuster V, Rydén LE, Cannom DS, et al (2006) ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): Developed in Collaboration With the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.106.177292
- January CT, Wann LS, Alpert JS, et al (2014) 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. https://doi.org/10.1161/CIR.0000000000000041
- January CT, Wann LS, Calkins H, et al (2019) 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. https://doi.org/10.1161/CIR.0000000000000665
- Developed with the special contribution of the European Heart Rhythm Association (EHRA), Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS), Authors/Task Force Members, et al (2010) Guidelines for the management of atrial fibrillation: The Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). European Heart Journal 31:2369–2429
- Hindricks G, Potpara T, Dagres N, et al (2021) 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal 42:373–498
- Lip GYH, Collet JP, Caterina RD, et al (2017) Antithrombotic therapy in atrial fibrillation associated with valvular heart disease: a joint consensus document from the European Heart Rhythm Association (EHRA) and European Society of Cardiology Working Group on Thrombosis, endorsed by the ESC Working Group on Valvular Heart Disease, Cardiac Arrhythmia Society of Southern Africa (CASSA), Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), South African Heart (SA Heart) Association and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLEACE). EP Europace 19:1757–1758
- Otto CM, Nishimura RA, Bonow RO, et al (2021) 2020 ACC/AHA guideline for the management of patients with valvular heart disease. The Journal of Thoracic and Cardiovascular Surgery 162:e183–e353
- Vahanian A, Beyersdorf F, Praz F, et al (2022) 2021 ESC/EACTS Guidelines for the management of valvular heart disease. European Heart Journal 43:561–632
- Lip GYH, Jensen M, Melgaard L, Skjøth F, Nielsen PB, Larsen TB (2019) Stroke and bleeding risk scores in patients with atrial fibrillation and valvular heart disease: evaluating ‘valvular heart disease’ in a nationwide cohort study. EP Europace 21:33–40
- Dipiro JT, Yee GC, Haines ST, Nolin TD, Ellingrod VL, Posey LM (2023) Chapter 40, Arrhythmia, DiPiro’s Pharmacotherapy: A Pathophysiologic Approach. McGraw Hill Medical
- Kanuri SH, Kreutz RP (2019) Pharmacogenomics of Novel Direct Oral Anticoagulants: Newly Identified Genes and Genetic Variants. JPM 9:7
- PubChem (S)-Warfarin. https://pubchem.ncbi.nlm.nih.gov/compound/54688261. Accessed 13 May 2023.
- PubChem (R)-Warfarin. https://pubchem.ncbi.nlm.nih.gov/compound/54684598. Accessed 13 May 2023.
- PubChem Dabigatran Etexilate. https://pubchem.ncbi.nlm.nih.gov/compound/135565674. Accessed 13 May 2023.
- PubChem Dabigatran Ethyl Ester. https://pubchem.ncbi.nlm.nih.gov/compound/446804. Accessed 13 May 2023.
- PubChem Dabigatran. https://pubchem.ncbi.nlm.nih.gov/compound/216210.Accessed 13 May 2023.
- DailyMed - WARFARIN SODIUM tablet. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=c90be37c-0ad0-4ccd-8fe7-b9a3427f0d80.Accessed 13 May 2023.
- Hirsh J, Fuster V, Ansell J, Halperin JL, American Heart Association/American College of Cardiology Foundation. American Heart Association/American College of Cardiology Foundation guide to warfarin therapy. J Am Coll Cardiol. 2003;41(9):1633-1652. doi:10.1016/s0735-1097(03)00416-9
- Jain N, Reilly RF. Clinical pharmacology of oral anticoagulants in patients with kidney disease. Clin J Am Soc Nephrol. 2019;14(2):278-287. doi:10.2215/CJN.02170218
- Steffel J, Verhamme P, Potpara TS, et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39(16):1330-1393. doi:10.1093/eurheartj/ehy136
- DailyMed - PRADAXA- dabigatran etexilate mesylate capsule. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=ba74e3cd-b06f-4145-b284-5fd6b84ff3c9. Accessed 13 May 2023.
- Lip GYH, Banerjee A, Boriani G, et al (2018) Antithrombotic Therapy for Atrial Fibrillation. Chest 154:1121–1201
- Tan CSS, Lee SWH (2021) Warfarin and food, herbal or dietary supplement interactions: A systematic review. Brit J Clinical Pharma 87:352–374
- Schaefer JK, McBane RD, Wysokinski WE (2016) How to choose appropriate direct oral anticoagulant for patient with nonvalvular atrial fibrillation. Ann Hematol 95:437–449
- Page MJ, McKenzie JE, Bossuyt PM, et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ n71
- Schulman S, Kearon C (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non‐surgical patients. Journal of Thrombosis and Haemostasis 3:692–694
- Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC. Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
- Risk of bias tools - Current version of RoB 2. https://www.riskofbias.info/welcome/rob-2-0-tool/current-version-of-rob-2. Accessed 30 May 2023
- Deeks JJ (2002) Issues in the selection of a summary statistic for meta‐analysis of clinical trials with binary outcomes. Statistics in Medicine 21:1575–1600
- Poole C, Shrier I, VanderWeele TJ (2015) Is the Risk Difference Really a More Heterogeneous Measure?: Epidemiology 26:714–718
- Higgins JPT, Li T, Deeks JJ (editors). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
- Borenstein M, Higgins JP, Hedges LV, Rothstein HR. Basics of meta-analysis: I²is not an absolute measure of heterogeneity. Res Synth Methods. 2017 Mar;8(1):5-18.
- Borenstein M (2019) Common mistakes in meta-analysis and how to avoid them. Biostat, Inc, Englewood, NJ
- Borenstein M (2023) How to understand and report heterogeneity in a meta-analysis: The difference between I-squared and prediction intervals. Integrative Medicine Research 12:101014
- Borenstein, M., Hedges, L. E., Higgins, J. P. T., & Rothstein, H. R. (2022). Comprehensive Meta-Analysis Version 4. In Biostat, Inc. www.Meta-Analysis.com
- Connolly SJ, Ezekowitz MD, Yusuf S, et al (2009) Dabigatran versus Warfarin in Patients with Atrial Fibrillation. N Engl J Med 361:1139–1151
- Ezekowitz MD, Reilly PA, Nehmiz G, Simmers TA, Nagarakanti R, Parcham-Azad K, Pedersen KE, Lionetti DA, Stangier J, Wallentin L (2007) Dabigatran With or Without Concomitant Aspirin Compared With Warfarin Alone in Patients With Nonvalvular Atrial Fibrillation (PETRO Study). The American Journal of Cardiology 100:1419–1426
- Cannon CP, Bhatt DL, Oldgren J, et al (2017) Dual Antithrombotic Therapy with Dabigatran after PCI in Atrial Fibrillation. N Engl J Med 377:1513–1524
- Cho MS, Kim M, Lee S, et al (2022) Comparison of Dabigatran Versus Warfarin Treatment for Prevention of New Cerebral Lesions in Valvular Atrial Fibrillation. The American Journal of Cardiology 175:58–64
- Calkins H, Willems S, Gerstenfeld EP, et al (2017) Uninterrupted Dabigatran versus Warfarin for Ablation in Atrial Fibrillation. N Engl J Med 376:1627–1636
- Nogami A, Harada T, Sekiguchi Y, et al (2019) Safety and Efficacy of Minimally Interrupted Dabigatran vs Uninterrupted Warfarin Therapy in Adults Undergoing Atrial Fibrillation Catheter Ablation: A Randomized Clinical Trial. JAMA Netw Open 2:e191994
- Eikelboom JW, Connolly SJ, Brueckmann M, et al (2013) Dabigatran versus Warfarin in Patients with Mechanical Heart Valves. N Engl J Med 369:1206–1214
- Durães AR, De Souza Roriz P, De Almeida Nunes B, Albuquerque FPE, De Bulhões FV, De Souza Fernandes AM, Aras R (2016) Dabigatran Versus Warfarin After Bioprosthesis Valve Replacement for the Management of Atrial Fibrillation Postoperatively: DAWA Pilot Study. Drugs R D 16:149–154
- Clinicaltrials.gov. In: Clinicaltrials.gov. https://clinicaltrials.gov/ct2/show/results/NCT01136408. Accessed 13 May 2023
- Ezekowitz MD, Nagarakanti R, Noack H, et al (2016) Comparison of Dabigatran and Warfarin in Patients With Atrial Fibrillation and Valvular Heart Disease: The RE-LY Trial (Randomized Evaluation of Long-Term Anticoagulant Therapy). Circulation 134:589–598
- Nin T, Sairaku A, Yoshida Y, Kamiya H, Tatematsu Y, Nanasato M, Inden Y, Hirayama H, Murohara T (2013) A Randomized Controlled Trial of Dabigatran versus Warfarin for Periablation Anticoagulation in Patients Undergoing Ablation of Atrial Fibrillation. Pacing Clinical Electrophis 36:172–179
- Pan K, Singer DE, Ovbiagele B, Wu Y, Ahmed MA, Lee M (2017) Effects of Non–Vitamin K Antagonist Oral Anticoagulants Versus Warfarin in Patients With Atrial Fibrillation and Valvular Heart Disease: A Systematic Review and Meta‐Analysis. JAHA 6:e005835
- De Souza Lima Bitar Y, Neto MG, Filho JAL, Pereira LV, Travassos KSO, Akrami KM, Roever L, Duraes AR (2019) Comparison of the New Oral Anticoagulants and Warfarin in Patients with Atrial Fibrillation and Valvular Heart Disease: Systematic Review and Meta-Analysis. Drugs R D 19:117–126
- Batool S, Chaudhari SS, Shaik TA, Dhakal S, Ahmad Ganaie Z, Ghaffari MAZ, Saleem F, Khan A (2022) Comparison of Direct Oral Anticoagulants and Warfarin in the Prevention of Stroke in Patients With Valvular Heart Disease: A Meta-Analysis. Cureus. https://doi.org/10.7759/cureus.28763
- Waranugraha Y, Rizal A, Syaban MFR, Faratisha IFD, Erwan NE, Yunita KC (2021) Direct comparison of non-vitamin K antagonist oral anticoagulant versus warfarin for stroke prevention in non-valvular atrial fibrillation: a systematic review and meta-analysis of real-world evidences. Egypt Heart J 73:70
- Yu Y, Liu J, Fu G, Fang R, Gao F, Chu H (2018) Comparison of dabigatran and warfarin used in patients with non-valvular atrial fibrillation: Meta-analysis of random control trial. Medicine 97:e12841
- Developed with the special contribution of the European Heart Rhythm Association (EHRA), Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS), Authors/Task Force Members, et al (2010) Guidelines for the management of atrial fibrillation: The Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). European Heart Journal 31:2369–2429
- Ahmad S, Wilt H (2016) Stroke Prevention in Atrial Fibrillation and Valvular Heart Disease. TOCMJ 10:110–116
- Kim JY, Kim S-H, Myong J-P, Kim YR, Kim T-S, Kim J-H, Jang S-W, Oh Y-S, Lee MY, Rho T-H (2019) Outcomes of Direct Oral Anticoagulants in Patients With Mitral Stenosis. Journal of the American College of Cardiology 73:1123–1131
- Mumoli N, Amellone C, Antonelli G, et al (2020) Clinical Discussions in Antithrombotic Therapy Management in Patients With Atrial Fibrillation: A Delphi Consensus Panel. CJC Open 2:641–651
- Diyarbakir T, Guzel T, Aktan A (2022) Oral Anticoagulant Use and Long-Term Follow-Up Results in Patients with Non-valvular Atrial Fibrillation in Turkey AFTER-2 Study. The Anatolian Journal of Cardiology 26:567–576
- Pastori D, Menichelli D, Cammisotto V, Pignatelli P (2021) Use of Direct Oral Anticoagulants in Patients With Antiphospholipid Syndrome: A Systematic Review and Comparison of the International Guidelines. Front Cardiovasc Med 8:715878
- Lip GYH, Keshishian AV, Zhang Y, et al (2021) Oral Anticoagulants for Nonvalvular Atrial Fibrillation in Patients With High Risk of Gastrointestinal Bleeding. JAMA Netw Open 4:e2120064
- By the 2023 American Geriatrics Society Beers Criteria® Update Expert Panel (2023) American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J American Geriatrics Society 71:2052–2081
- Connolly SJ, Wallentin L, Ezekowitz MD, et al (2013) The Long-Term Multicenter Observational Study of Dabigatran Treatment in Patients With Atrial Fibrillation (RELY-ABLE) Study. Circulation 128:237–243
- Jansson M, Själander S, Sjögren V, Björck F, Renlund H, Norrving B, Själander A (2023) Reduced dose direct oral anticoagulants compared with warfarin with high time in therapeutic range in nonvalvular atrial fibrillation. J Thromb Thrombolysis 55:415–425
- Mannacio VA, Mannacio L, Antignano A, Mauro C, Mastroroberto P, Musumeci F, Zebele C, Iannelli G (2022) New Oral Anticoagulants Versus Warfarin in Atrial Fibrillation After Early Postoperative Period in Patients With Bioprosthetic Aortic Valve. The Annals of Thoracic Surgery 113:75–82
- Russo V, Carbone A, Attena E, et al (2019) Clinical Benefit of Direct Oral Anticoagulants Versus Vitamin K Antagonists in Patients with Atrial Fibrillation and Bioprosthetic Heart Valves. Clinical Therapeutics 41:2549–2557
- Duan L, Doctor JN, Adams JL, Romley JA, Nguyen L-A, An J, Lee M-S (2021) Comparison of Direct Oral Anticoagulants Versus Warfarin in Patients With Atrial Fibrillation and Bioprosthetic Heart Valves. The American Journal of Cardiology 146:22–28
- Myllykangas ME, Kiviniemi TO, Gunn JM, Salomaa VV, Pietilä A, Niiranen TJ, Aittokallio J (2021) Anticoagulation Therapy After Biologic Aortic Valve Replacement. Front Cardiovasc Med 8:698784
- Mentias A, Saad M, Michael M, et al (2022) Direct Oral Anticoagulants Versus Warfarin in Patients With Atrial Fibrillation and Valve Replacement or Repair. JAHA 11:e026666
- Yadlapati A, Groh C, Malaisrie SC, Gajjar M, Kruse J, Meyers S, Passman R (2016) Efficacy and safety of novel oral anticoagulants in patients with bioprosthetic valves. Clin Res Cardiol 105:268–272
- Russo V, Attena E, Mazzone C, Esposito F, Parisi V, Bancone C, Rago A, Nigro G, Sangiuolo R, D’ Onofrio A (2018) Nonvitamin K Antagonist Oral Anticoagulants Use in Patients with Atrial Fibrillation and Bioprosthetic Heart Valves/Prior Surgical Valve Repair: A Multicenter Clinical Practice Experience. Semin Thromb Hemost 44:364–369
- Yamaji H, Murakami T, Hina K, Higashiya S, Kawamura H, Murakami M, Kamikawa S, Hirohata S, Kusachi S (2013) Usefulness of Dabigatran Etexilate as Periprocedural Anticoagulation Therapy for Atrial Fibrillation Ablation. Clin Drug Investig 33:409–418