Comparative Analysis of Dietary Habits and Nutritional Profiles: Sidi Ali Ben Aoun vs. Grand Tunis
##plugins.themes.academic_pro.article.main##
Abstract
Introduction: Tunisia is affected by the nutritional and dietary transition.
Aim: To compare dietary habits and nutritional profiles between a rural agricultural area Sidi Ali Ben Aoun and an urban area Grand Tunis.
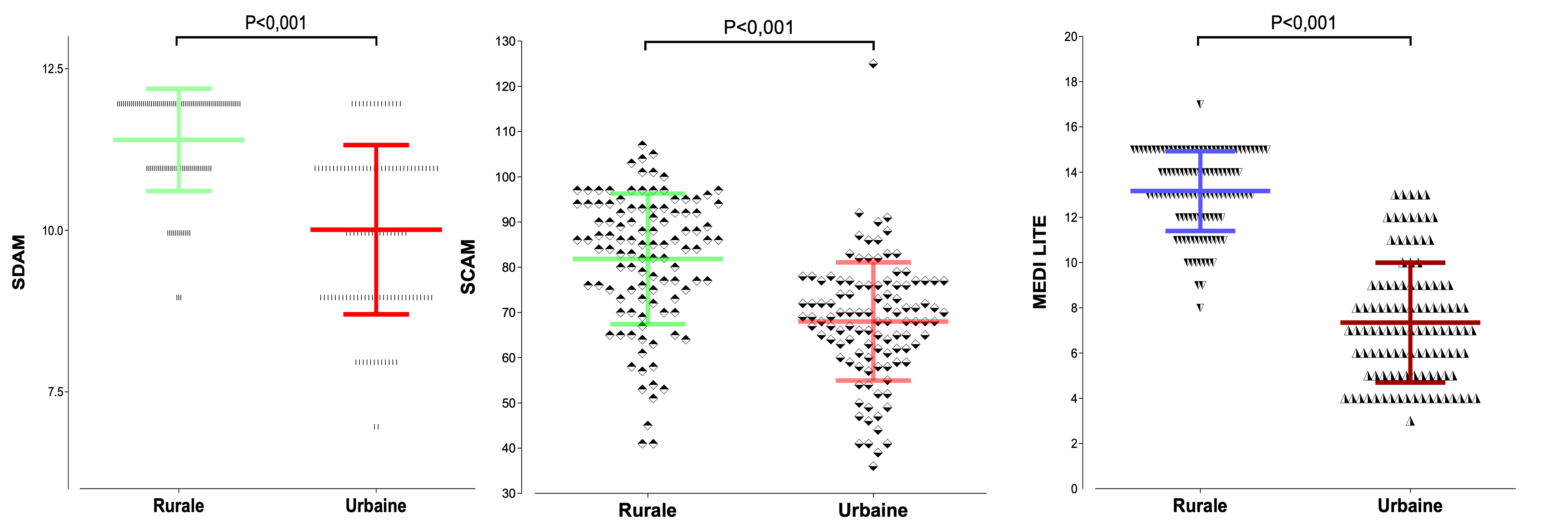
Methods: This is a comparative cross-sectional study conducted on a sample of 220 participants, including 110 from Ben Aoun and 110 from Grand Tunis. Data were collected based on a pre-established questionnaire about dietary lifestyle and habits survey. Validated scores were used: Alimentary Diversity of Households (SDAM), the Food Consumption Assessment score (SCAM), MEDI-LITE and IPAQ.
Results: The mean age was 37.2±15.3 years for the urban population versus 38.7±13.8 years for the rural population (p=0.43). In the rural population, males were 54.5% vs 48.2%; p=0.34. The occurrence of non-communicable diseases was lower in Ben Aoun (p<0.001). The adopted diet in the region of Ben Aoun aligned with the principles of the Mediterranean diet (MEDI-LITE score was 13.2±1.76 versus 7.35±2.65 in Grand Tunis, p<0.001). Both studied regions had a similar level of food security as assessed by the SDAM (p=0.006). However, household dietary diversity was more present in the rural region: the average SCAM was 11.4±0.79 in the rural group compared to 10±1.31 in the urban group (p<0.001).
Conclusion: The rural region (Sidi Ali Ben Aoun) was characterized by a healthier and more diverse diet compared to the urban region (Grand Tunis).
Keywords:
nutritional transition, dietary habits, mediterranean diet, food security, alimentary diversity##plugins.themes.academic_pro.article.details##

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
- Bellundagi V, Umesh KB, Ashwini BC, von Cramon-Taubadel S. Crop Diversity, Dietary Diversity, and Nutritional Intake: Evidence on Inter-Linkages Across the Rural–Urban Interface of Bengaluru. In: Hoffmann E, Buerkert A, von Cramon-Taubadel S, Umesh KB, Pethandlahalli Shivaraj P, Vazhacharickal PJ, editors. The Rural-Urban Interface: An Interdisciplinary Research Approach to Urbanisation Processes Around the Indian Megacity Bengaluru, Cham: Springer International Publishing; 2021, p. 111–7. https://doi.org/10.1007/978-3-030-79972-4_11.
- Haysom G. Food and the City: Urban Scale Food System Governance. Urban Forum 2015;26:263–81. https://doi.org/10.1007/s12132-015-9255-7.
- Popkin BM. The nutrition transition in low-income countries: an emerging crisis. Nutr Rev 1994;52:285–98. https://doi.org/10.1111/j.1753-4887.1994.tb01460.x.
- Maire B, Lioret S, Gartner A, Delpeuch F. Transition nutritionnelle et maladies chroniques non transmissibles liées à l’alimentation dans les pays en développement. Cahiers d’études et de Recherches Francophones / Santé 2002;12:45–55.
- Tomioka K, Iwamoto J, Saeki K, Okamoto N. Reliability and validity of the International Physical Activity Questionnaire (IPAQ) in elderly adults: the Fujiwara-kyo Study. J Epidemiol 2011;21:459–65. https://doi.org/10.2188/jea.je20110003.
- Somé JW, Jones AD. The influence of crop production and socioeconomic factors on seasonal household dietary diversity in Burkina Faso. PLoS One 2018;13:e0195685. https://doi.org/10.1371/journal.pone.0195685.
- Dinu M, Pagliai G, Lotti S, Giangrandi I, Colombini B, Sofi F. Adherence to Mediterranean Diet Measured through Medi-Lite Score and Obesity: A Retrospective Study. Nutrients 2021;13:2007. https://doi.org/10.3390/nu13062007.
- Sofi F, Dinu M, Pagliai G, Marcucci R, Casini A. Validation of a literature-based adherence score to Mediterranean diet: the MEDI-LITE score. Int J Food Sci Nutr 2017;68:757–62. https://doi.org/10.1080/09637486.2017.1287884.
- Kamoun M, Hajem S, Imen S, Achour N, Slimane H. Prevalence of obesity and overweight in Tunisia on 2001. Tunis Med 2008;86:649–52.
- Boukli Hacène L, Khelil M-A, Chabane Sari D, Meguenni K, Meziane Tani A. [Prevalence of cardiovascular risk factors in urban and rural communities in the Wilaya of Tlemcen (Algeria): A comparative study]. Rev Epidemiol Sante Publique 2017;65:277–84. https://doi.org/10.1016/j.respe.2017.01.121.
- Jaffiol C. Le diabète sucré en Afrique : un enjeu de santé publique. Bulletin de l’Académie Nationale de Médecine 2011;195:1239–54. https://doi.org/10.1016/S0001-4079(19)31983-1.
- Deblij S, Bahlaouan B, Boutaleb N, Boutaleb F, Bennani M, El Antri S. The Urban Development in Relation to the Occurrence of Diseases in the Casa-Settat Region of Morocco during the Emergence of SARS-CoV-2. ScientificWorldJournal 2022;2022:1093956. https://doi.org/10.1155/2022/1093956.
- Miossec J-M. Urbanisation des campagnes et ruralisation des villes en Tunisie 1985. https://doi.org/10.3406/geo.1985.20300.
- Chen SE, Florax RJ, Snyder SD. Obesity and fast food in urban markets: a new approach using geo-referenced micro data. Health Economics 2013;22:835–56. https://doi.org/10.1002/hec.2863.
- Sharkey JR, Johnson CM, Dean WR, Horel SA. Association between proximity to and coverage of traditional fast-food restaurants and non-traditional fast-food outlets and fast-food consumption among rural adults. International Journal of Health Geographics 2011;10:37. https://doi.org/10.1186/1476-072X-10-37.
- Diakite D. Évolution de la consommation alimentaire des adultes de 35 à 70 ans sur une décennie en Tunisie (1996-2005) : facteurs sociodémographiques, économiques et environnementaux associés 2019.
- Siri JG, Newell B, Proust K, Capon A. Urbanization, Extreme Events, and Health: The Case for Systems Approaches in Mitigation, Management, and Response. Asia Pac J Public Health 2016;28:15S-27S. https://doi.org/10.1177/1010539515595694.
- Adetola OY, Taylor JRN, Duodu KG. Can consumption of local micronutrient- and absorption enhancer-rich plant foods together with starchy staples improve bioavailable iron and zinc in diets of at-risk African populations? Int J Food Sci Nutr 2023;74:188–208. https://doi.org/10.1080/09637486.2023.2182740.
- Sg M, Mw Q. Vegetables. Advances in Neurobiology 2020;24. https://doi.org/10.1007/978-3-030-30402-7_9.
- Gatton ML, Gallegos D. A 5-year review of prevalence, temporal trends and characteristics of individuals experiencing moderate and severe food insecurity in 34 high income countries. BMC Public Health 2023;23:2215. https://doi.org/10.1186/s12889-023-17139-9.
- Kota K, Chomienne M-H, Yaya S. Examining the disparities: A cross-sectional study of socio-economic factors and food insecurity in Togo. PLoS One 2023;18:e0294527. https://doi.org/10.1371/journal.pone.0294527.
- Miller KR, Jones CM, McClave SA, Christian V, Adamson P, Neel DR, et al. Food Access, Food Insecurity, and Gun Violence: Examining a Complex Relationship. Curr Nutr Rep 2021;10:317–23. https://doi.org/10.1007/s13668-021-00378-w.
- Ganpule A, Brown KA, Dubey M, Srinivasapura Venkateshmurthy N, Jarhyan P, Maddury AP, et al. Food insecurity and its determinants among adults in North and South India. Nutr J 2023;22:2. https://doi.org/10.1186/s12937-022-00831-8.
- El Rhazi K, Nejjari C, Romaguera D, Feart C, Obtel M, Zidouh A, et al. Adherence to a Mediterranean diet in Morocco and its correlates: cross-sectional analysis of a sample of the adult Moroccan population. BMC Public Health 2012;12:345. https://doi.org/10.1186/1471-2458-12-345.
- Kiani AK, Medori MC, Bonetti G, Aquilanti B, Velluti V, Matera G, et al. Modern vision of the Mediterranean diet. J Prev Med Hyg 2022;63:E36–43. https://doi.org/10.15167/2421-4248/jpmh2022.63.2S3.2745.