Postpartum Septic Osteoarthritis: A case series study
##plugins.themes.academic_pro.article.main##
Abstract
Introduction-Aim: Postpartum septic osteoarthritis is a rare but serious condition often misdiagnosed due to overlap with common postpartum symptoms like pelvic pain and joint stiffness. This case series aims to describe the clinical, bacteriological, and radiological characteristics of postpartum septic osteoarthritis, as well as the treatment approaches and patient outcomes.
Methods: A retrospective case series was conducted at Farhat Hached University Hospital, from 2006 to 2022, involving patients with confirmed postpartum septic osteoarthritis. Clinical data, laboratory findings, imaging results, treatments, and outcomes were analyzed
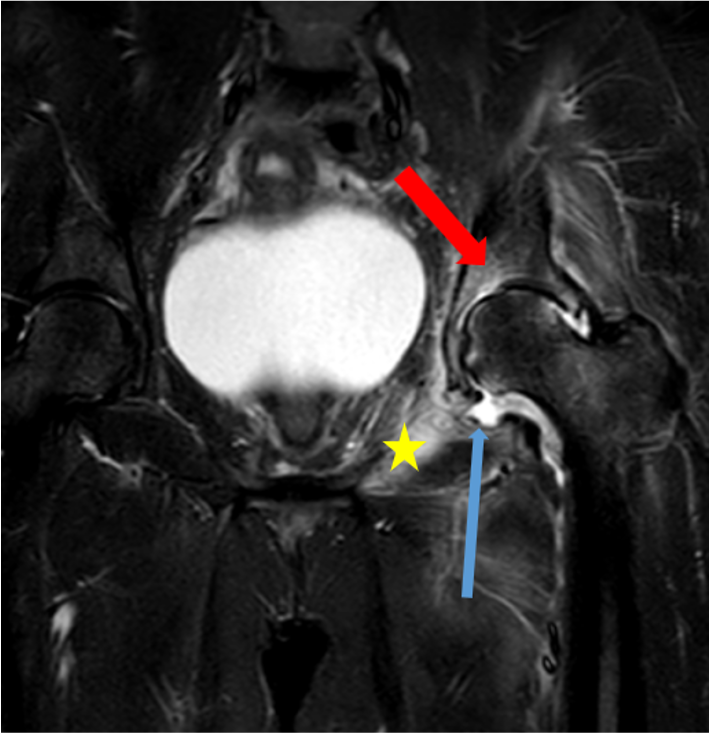
Results: The mean age of the seven patients was 31.4 years. All patients presented with joint pain, with fever and functional impairment where each was observed in 85.7% of cases. The average diagnostic delay was 17 days. MRI findings revealed bone marrow edema in all patients, Abscesses in 28.5% of cases, periarticular soft tissue edema, and intra-articular effusions in 71.4% of cases. The pubic symphysis was the most commonly affected site (57.1%), followed by the sacroiliac joints (28.6%). Only one pathogen, Streptococcus pyogenes, was isolated. Nearly all patients received dual antibiotic therapy for an average duration of 4 to 6 weeks. Satisfactory clinical progress without sequelae was noted and maintained after an average follow-up of 5 to 6 months.
Conclusion: Our results revealed that postpartum septic osteoarthritis requires prompt diagnosis and early treatment to prevent severe complications. MRI plays a critical role in early detection, while timely antibiotic therapy leads to favorable long-term outcomes
Keywords:
Postpartum, septic osteoarthritis, MRI, treatment, outcome, diagnosis##plugins.themes.academic_pro.article.details##

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
- Vinceneux P, Rist S, Bosquet A. Arthrites septiques des sacro-iliaques et de la symphyse pubienne. Rev Rhum. 2006;73(2):177‑82.
- Hermet M, Minichiello E, Flipo RM, Dubost JJ, Allanore Y, Ziza JM, et al. Infectious sacroiliitis: a retrospective, multicentre study of 39 adults. BMC Infect Dis. 2012;12:305‑11.
- Ross JJ, Hu LT. Septic arthritis of the pubic symphysis: review of 100 cases. Medicine (Baltimore). 2003;82(5):340‑5.
- Timsit MA. Grossesse et douleurs rhumatologiques lombaires basses et de la ceinture pelvienne. Gynécologie Obstétrique Fertil. 2004;32(5):420‑6.
- Prestinaci F, Pezzotti P, Pantosti A. Antimicrobial resistance: a global multifaceted phenomenon. Pathog Glob Health. 2015;109(7):309-18
- Belfort MA, Clark SL, Saade GR, Kleja K, Dildy GA, Van Veen TR, Akhigbe E, Frye DR, Meyers JA, Kofford S. Hospital readmission after delivery: evidence for an increased incidence of nonurogenital infection in the immediate postpartum period. Am J Obstet Gynecol. 2010 Jan;202(1):35.e1-7.
- Tsoi C, Griffith JF, Lee RKL, Wong PCH, Tam LS. Imaging of sacroiliitis: Current status, limitations and pitfalls. Quant Imaging Med Surg. 2019;9(2):318‑35.
- Malghem J, Vande Berg B, Lecouvet F, Koutaissoff S, Maldague B. Principes d’interpretation de l’imagerie des articulations sacro-iliaques. JBR-BTR Organe Soc R Belge Radiol SRBR Orgaan Van K Belg Ver Voor Radiol KBVR. 2007;90(5):358‑67.
- Vale-Fernandes E, Rodrigues F, Monteiro C, Carvalho L. Infectious Postpartum Sacroiliitis: The Importance and Difficulty of Early Diagnosis. Acta Med Port. 2016;29(7‑8):484‑7.
- Millwala F, Chen S, Tsaltskan V, Simon G. Acupuncture and postpartum pyogenic sacroiliitis: a case report. J Med Case Reports. 2015;9:193‑5.
- Maier SP, Wixted JJ. Native Hip Septic Arthritis in the Setting of Postpartum Gynecologic Infection: A Case Report. JBJS Case Connect. 2021;11(2):979‑83.
- Phuah CL, Javid B, Aliyu SH, Lever AML. A case of Mycoplasma hominis septic arthritis postpartum. J Infect. 2007;55(5):135‑7.
- Almoujahed MO, Khatib R, Baran J. Pregnancy-associated pyogenic sacroiliitis: case report and review. Infect Dis Obstet Gynecol. 2003;11(1):53‑7
- Balato G, de Matteo V, Ascione T, de Giovanni R, Marano E, Rizzo M, et al. Management of septic arthritis of the hip joint in adults. A systematic review of the literature. BMC Musculoskelet Disord. 2021;22(Suppl 2):1006.
- Stürzenbecher A, Braun J, Paris S, Biedermann T, Hamm B, Bollow M. MR imaging of septic sacroiliitis. Skeletal Radiol. 2000;29(8):439‑46.
- Tuite MJ. Sacroiliac joint imaging. In: Seminars in musculoskeletal radiology. © Thieme Medical Publishers; 2008. p. 72‑82.
- Abid H, Chaabouni S, Frikha F, Toumi N, Souissi B, Lahiani D, et al. Apport de l’imagerie dans le diagnostic des sacroiliites infectieuses : à propos de 19 cas. Pan Afr Med J. 2014;17:171‑6.
- Bellussi A, Busi Rizzi E, Schininà V, De Santis A, Bibbolino C. STIR sequence in infectious sacroiliitis in three patients. Clin Imaging. 2002;26(3):212‑5.
- Imagama T, Tokushige A, Sakka A, Seki K, Taguchi T. Postpartum pyogenic sacroiliitis with methicillin-resistant Staphylococcus aureus in a healthy adult: A case report and review of the literature. Taiwan J Obstet Gynecol. 2015;54(3):303‑5.